If your organization is involved in the healthcare industry indirectly, such as through strategic partnerships with healthcare providers, you may be required to sign a business associate agreement. That means achieving partial or full HIPAA compliance through implementation and assessments.
HIPAA / Healthcare Industry
If your organization needs to comply with HIPAA, you’ll need to keep an eye out for:
- Identifiable records related to patients’ health conditions
- Identifiable records related to the provision of healthcare services
- Identifiable records related to payments for healthcare provided
- Methods for de-identifying PHI to lessen the scope of compliance
- Approaches to comprehensive HIPAA compliance implementation
The development and advancement of cloud computing services have improved and expanded technology options across several industries. The healthcare industry is no exception. Due to legal regulations, organizations in and adjacent to healthcare have unique cloud infrastructure security considerations to prioritize to safeguard specific classes of protected information.
Complying with HIPAA regulations is as easy as following four simple steps:
- Determining whether your organization is considered a covered entity
- Implementing controls for the prescriptive HIPAA rules
- Ensuring you have the infrastructure for breach notification
- Streamlining compliance requirements with a unified approach
From the largest hospitals in America to dentists and plastic surgeons, virtually everyone in the medical profession or anyone that deals with public health is affected by the Health Insurance Portability and Accountability Act (HIPAA). HIPAA is the law of the land as it relates to standards for patient private data and medical record privacy, and non-compliance and HIPAA violations can come with stiff penalties.
Most people would agree that basic human rights include privacy. However, social media, computers, and the Internet have eroded the traditional privacy and security barriers put in place. Documents can be shared with a simple click and access granted with credentials. Society can no longer dictate, in many cases, who or what has access to Personal Identifiable Information (PII).This especially affects healthcare provider entities, which up until the late 1990s and early 2000s kept most records in paper format.
Businesses both within and adjacent to healthcare need to comply with the HIPAA data security requirements, which may see changes in 2024. To protect your company from costly fines, you must store and protect patient data, while ensuring you have the necessary infrastructure to report breaches.
The Security Rule is one of the major prescriptive portions of the HIPAA regulation. It requires eligible companies, including those tangentially associated with healthcare organizations, to implement risk assessments and install a series of proactive safeguards that prevent and mitigate potential harm to PHI.
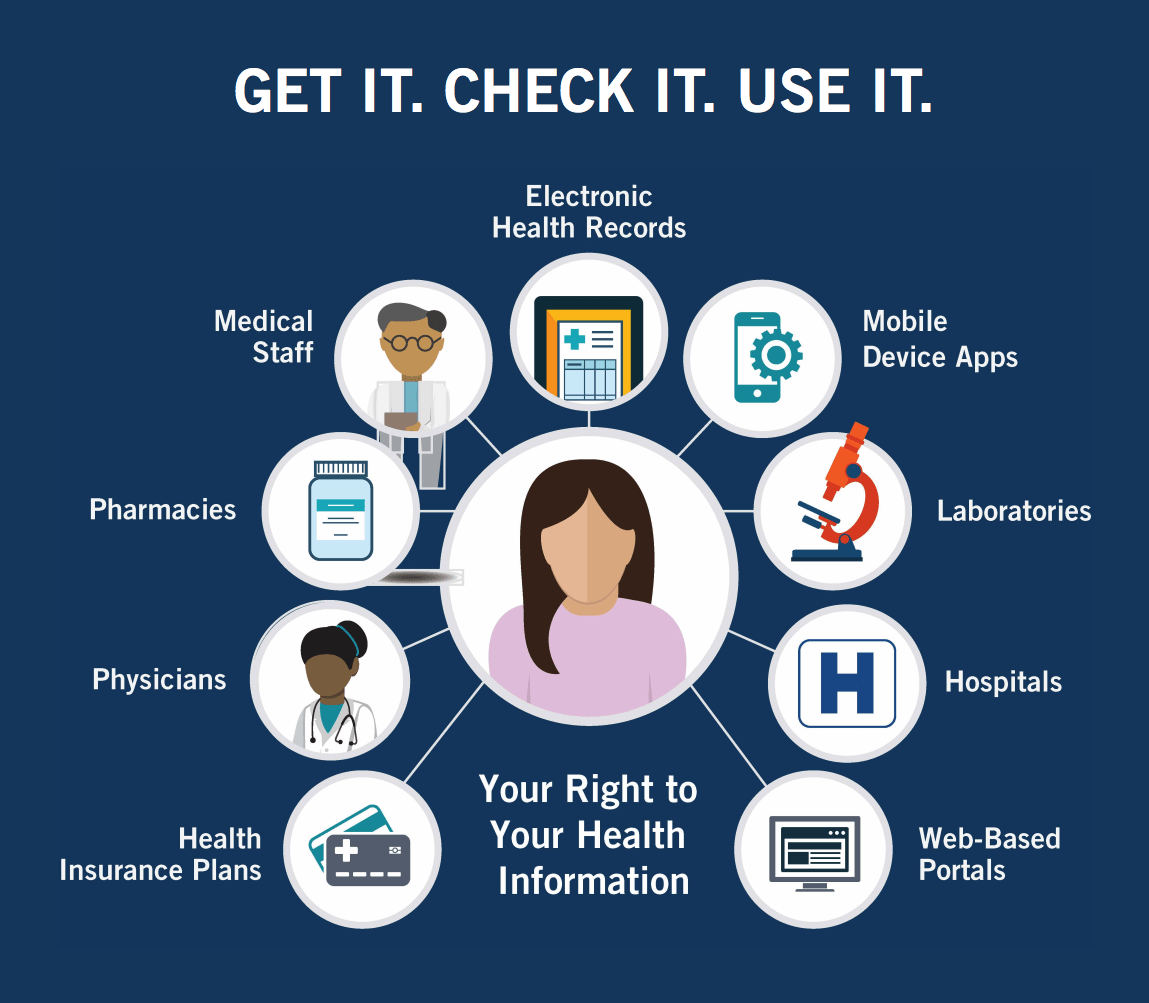
With an ever increasing level of connection between consumers and businesses, questions about privacy inevitably surface. This is especially apparent in the field of healthcare, where patients expect not only discretion by their providers, but also ease of access. 2016 data suggested younger generations would increasingly expect electronic (e.g., mobile devices) access to medical records. Likewise, a 2017 NRC Health report predicted consumers would expect transparency in the healthcare field. To balance patient privacy with these emerging trends, the Department of Health and Human Services (HHS) implemented the Health Insurance Portability and Accountability Act (HIPAA). To ensure your company is HIPAA compliant, check out our HIPAA guide and checklist below.
Whether your business is directly involved in healthcare or indirectly connected to the industry through trade, there’s a good chance you’ll need to comply with the Health Insurance Portability and Accountability Act of 1996 (HIPAA).